Guillain Barre Syndrome
Characteristics:
- Acute inflammatory demyelinating polyneuropathy
- It is a progressive ascending demyelinating disease of peripheral nervous system
- Disease process may progress from lung or GI infection (Campylobacter jejuni, Mycoplasma pneumoniae, CMV, EBV)
- It results in lower motor neuron paralysis
- Flaccid tendon reflex
- Organ involvement:
- Sudden onset of skeletal muscle paralysis or weakness
- Weakness begins at the legs and spread at the cephalic direction
- Symmetrical involvement
- Involves trunk, arms, face
- Cranial nerve involvement:
- Oculomotor nerves (CN III, IV, VI): diplopia
- Facial nerve (CN VII): bilateral facial weakness
- Bulbar nerves (CN IX and X): dysphagia and dysarthria
- Hypoglossal nerve (CN XII): tongue weakness
- Intercostal muscle paralysis ➔ inadequate ventilation
- Diaphragm palsy
- Sensory symptoms (numbness, tingling, pain) may also be present, but they are often less prominent.
Sensory abnormality may precede the motor weakness - Associated with pain
- Autonomic dysfunction
- Complete recovery within few weeks
Autonomic dysfunction in GBS is characterised by
➙ Fluctuation of blood pressure
➙ Orthostatic hypotension
➙ Impairment of normal compensatory vasoconstrictive response
➙ ↑ SVR
➙ Resting tachycardia
➙ Cardiac conduction abnormality
➙ Bradyarrhythmia and tachyarrhythmia may necessitate pacemaker insertion
➙ Sudden profuse diaphoresis
Diagnosis of autonomic dysfunction:
- Lack of respiratory variation in HR
- HR regularity
- Deep Breathing Test and Valsalva Maneuver
- Tilt Table Test
📌 Thromboembolism can occur due to immobility
📌 Sudden death is due to autonomic dysfunction (secondary to arrhythmia)
📌 Cause of death: Sepsis, acute respiratory failure, pulmonary embolism, sudden cardiac arrest
Pathophysiology:
➙ Autoimmune mediated or 1 - 4 week following URTI or GI infection with Campylobacter jejuni, CMV, EBV
➙ The target is myelin
➙ Axonal form may also occur
➙ Chronic inflammatory demyelinating neuropathy is continuum of GBS
Complication:
- Pulmonary infection
- Hyponatraemia
- Autonomic dysfunction
- Urinary tract infection
- Cognitive dysfunction
- Sepsis
- ARDS
- Pulmonary embolism
Investigation:
➙ CBC
➙ Urea, Electrolyte: SIADH may occur
➙ Liver & Renal function test: may be altered
➙ Clotting screening: abnormality to be excluded before plasmapheresis
➙ Ca2+: ↓ Ca may be exacerbated by plasmapheresis
➙ Antibody test: antiganglioside antibody, Antibodies to Campylobacter jejuni, cytomegalovirus, Epstein Barr virus, herpes simplex virus, Mycoplasma pneumoniae
➙ Brain CT: To exclude raised intracranial pressure or other causes of focal neurological signs prior to lumbar puncture
➙ Lumber puncture and CSF study: Typical findings in GBS are ↑ protein and cell count < 10/mm³
➙ Electrophysiological studies
➙ Gadolinium-enhanced MRI of the spinal cord: thickening of intrathecal nerve root Diagnosis:
- Progressive (over 2 - 4 weeks) symmetrical ascending bilateral weakness
- Areflexia
- Minor sensory symptoms
- Cranial nerve involvement
- Autonomic dysfunction
- ↑ CSF protein
- CSF cell count < 10/mm³
- Spontaneous recovery starts 2 - 4 weeks after a plateau phase of progression
Management:
➙ General care:
- Chest physiotherapy and passive limb movement
- Nasogastric feeding
- Stool softener
- Psychological support
- Prevention of thromboembolism
➙ Respiratory system:
- ABG to assess adequacy of ventilation and oxygenation
- Vital capacity is monitored 4 hourly, if < 15ml/kg, MV support is initiated
- Pharyngeal muscle weakness necessitates cuffed ET or TT even in the absence of respiratory failure
- Tracheostomy should be considered if prolonged MV is anticipated
➙ Cardiovascular system:
- Institution of MV may accompany hypotension
- Invasive BP monitoring
- Aggressive management of hypertension or hypotension due to ANS dysfunction
- Monitoring for ANS dysfunction
- Pacemaker if intractable bradyarrhythmia, β blocker for the rate control in tachycardia
Venous thromboembolism prophylaxis: Low molecular weight heparin in combination with either pneumatic compression devices or anti-embolism stockings, are recommended until patients are able to walk unaided.
➙ Neurological:
- Neuropathic pain is common
- Non-opioid analgesics (paracetamol) in combination with opioid analgesia should be instituted initially, but may provide inadequate pain relief.
- Adjunctive treatments such as anticonvulsants (gabapentin or carbemazepine) and tricyclic antidepressants may be effective.
➙ GIT:
- Patients with autonomic dysfunction may be susceptible to the development of a paralytic ileus.
- This may be treated with prokinetic agents such as metoclopramide or erythromycin.
- Good nutrition is important particularly for those patients with bulbar weakness, and those who are sedated and mechanically ventilated.
- Poor oral intake may necessitate instigation of enteral or parenteral feeding.
- Dietician input is useful to ensure adequate calorific, micronutrient, fluid and electrolyte intake.
➙ Immunemodulation:
- Corticosteroid
- It is not very much helpful
- Plasmapheresis:
- Plasma exchange is an effective treatment and accelerates recovery in GBS.
- Should be commenced within 2 weeks of the onset of illness
- Reduce duration of ventilator dependence and hospital stay
- Leads to earlier mobilisation
- Typically, up to 5 exchanges are performed substituting 250 ml kg–1 of plasma with 4.5% human albumin solution
- Contraindications to plasma exchange include:
- Coagulopathy
- Overwhelming sepsis
- Haemodynamic instability and shock
- Side effects:
- Nausea, vomiting, diarrhoea
- Fever
- Coagulopathy
- Immunosuppression
- Hypocalcaemia
- Intravenous immunoglobulin:
- IVIg contains pooled donor IgG antibodies and may reduce the severity of autoimmune inflammation in GBS by blocking Fc receptors. This prevents the Fc portion of antibodies binding and thus interrupts antibody mediated cell destruction. Complement activation is also altered.
- The recommended dose of intravenous immunoglobulin therapy is 0.4 mg/kg daily for 5–6 days
- Therapy should be commenced within 2 weeks of the onset of symptoms
- Contraindications to treatment include
- IgA deficiency (increased incidence of anaphylaxis)
- Previous anaphylaxis to immunoglobulin therapy
- IgA levels must be checked in all patients prior to administration of immunoglobulin
- Extreme caution must be taken in patients with renal impairment as renal function may deteriorate further with immunoglobulin therapy
- Side-effects:
- Nausea
- Fever
- Headache
- Transient rise in liver enzymes
- Encephalopathy, meningism and malaise
- Skin reactions (erythroderma)
- Hypercoagulability
- Deterioration in renal function due to renal tubular necrosis and anaphylaxis
Anaesthetic considerations:
➙ Abnormal ANS function
➙ Absence of compensatory cardiovascular response
- Profound hypotension with posture change, blood loss, PPV
- Exaggerated increase in blood pressure with laryngoscopy
➙ Presence of lower motor neuron disease
➙ Intercostal muscle paralysis ➔ inadequate ventilation, segmental lung collapse, ↓ lung compliance
➙ Bulbar palsy ➔ problem with sputum clearance and ↑ risk of aspiration
➙ Invasive BP monitoring is required
➙ Fatal response to suxamethonium
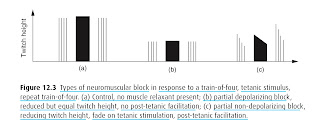
➙ Exaggerated response to nondepolarizing muscle relaxants
➙ Pain is difficult to treat
➙ Hyponatraemia due to inadequate secretion of ADH
➙ Chronic demyelinating polyneuropathy with a H/O GBS may exacerbate the anaesthetic effect with subsequent complications
Comments
Post a Comment
Please share your views and comments in the comment section. Give your opinion if there is anything to update.
Subscribe the channel to get updates regarding regular blog post.
Share the content if you think its appropriate.
Thank you.